Virus Going Around October 2024: The fall season often brings a surge in viral illnesses, and October 2024 is no exception. As temperatures cool and people spend more time indoors, viruses have an easier time spreading. This year, however, the viral landscape is a bit different, with new strains and variants emerging alongside familiar foes.
Understanding the viruses circulating in October 2024 is crucial for staying healthy and protecting yourself and your loved ones.
This article delves into the current viral landscape, exploring the most prevalent viruses, their symptoms, transmission methods, and effective prevention strategies. We’ll also discuss the impact of these viruses on public health, available vaccination and treatment options, and the importance of public awareness and education.
Contents List
- 1 Current Viral Landscape in October 2024
- 2 2. Symptoms and Transmission
- 3 Impact on Public Health
- 4 Vaccination and Treatment Options
- 5 6. Historical Context
- 6 7. Global Perspective
- 7 Future Considerations: Virus Going Around October 2024
- 8 9. Ethical Considerations
- 9 10. Social and Economic Impacts
- 10 11. Environmental Factors
- 10.1 Environmental Factors Influencing Viral Emergence and Spread
- 10.2 Impact of Climate Change on Viral Transmission
- 10.3 Deforestation and Habitat Fragmentation
- 10.4 Research on Environmental Factors and Viral Outbreaks
- 10.5 Environmental Factors and Viral Transmission
- 10.6 Scenario: Novel Virus Emergence in a Region with Environmental Changes
- 11 13. Research and Development
- 12 International Collaboration
- 13 Closing Notes
- 14 FAQ Insights
Current Viral Landscape in October 2024
October 2024 sees a continued presence of familiar respiratory viruses, alongside emerging strains and variants. While some viruses are experiencing seasonal peaks, others are showing a decline in activity compared to previous years. Understanding the current viral landscape is crucial for individuals and healthcare systems to prepare and respond effectively.
Prevalence of Viruses in October 2024
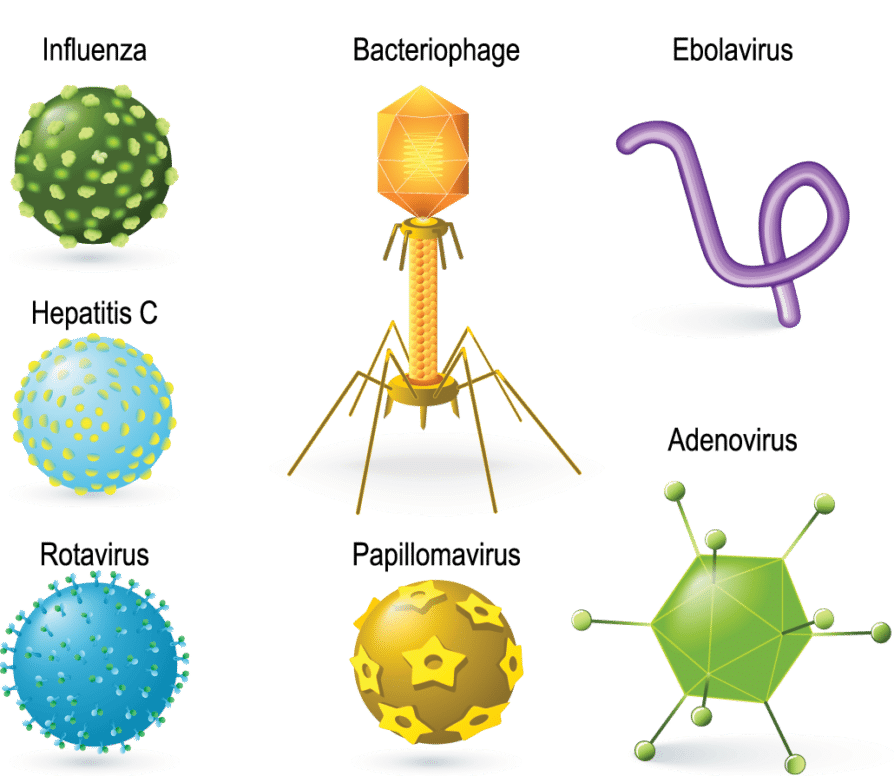
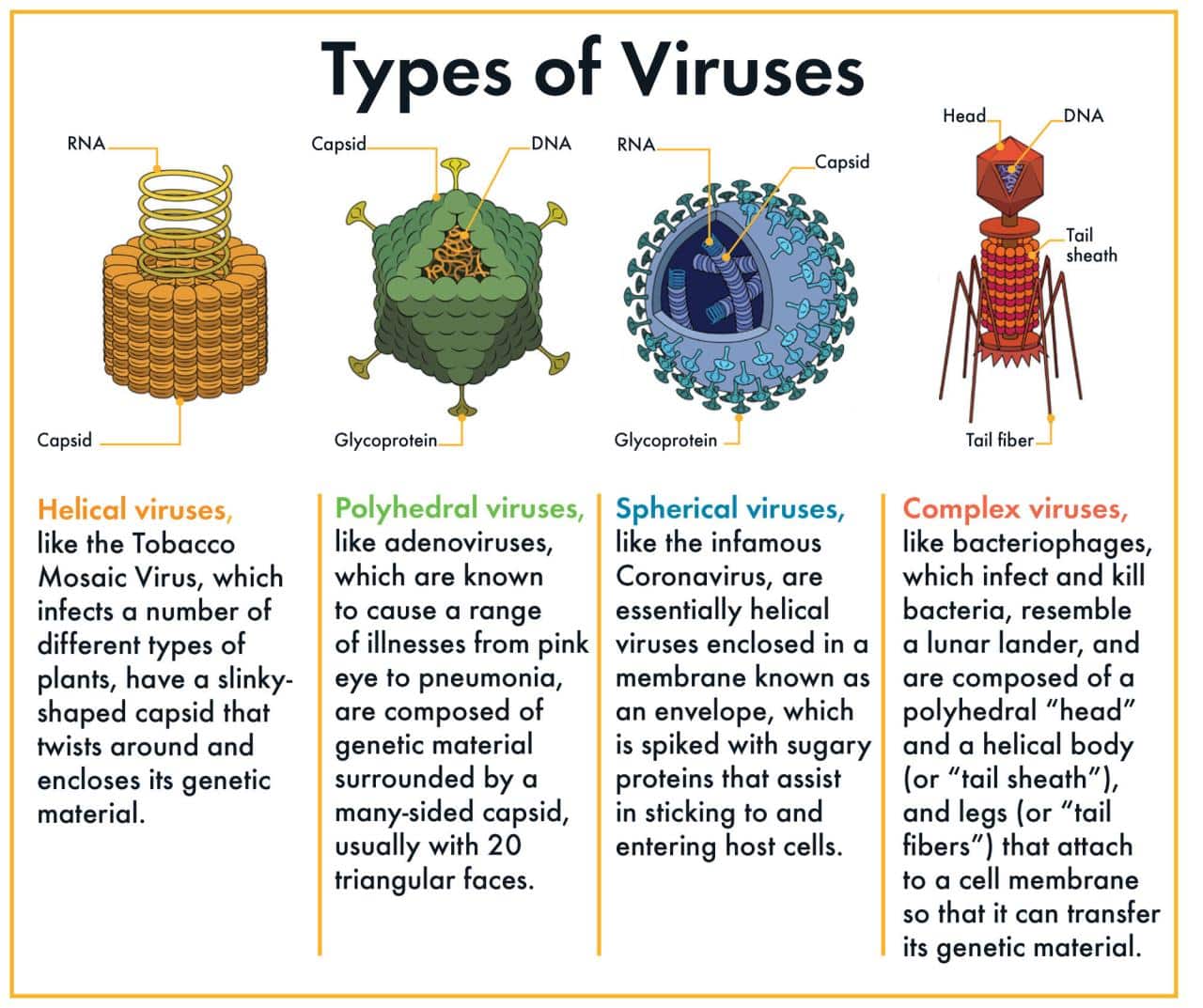
The most prevalent viruses circulating in October 2024 include:
- Influenza:Influenza A and B are expected to be circulating, with potential for seasonal peaks in October and November. Influenza activity in 2024 may be similar to previous years, with a slight increase in cases compared to 2023.
- Respiratory Syncytial Virus (RSV):RSV activity typically peaks in the fall and winter months, and October 2024 is likely to see a rise in cases, particularly among young children. Vaccination and preventative measures are recommended to reduce the risk of infection.
- Rhinoviruses:These common cold viruses are circulating year-round, with a slight increase in activity during the fall and winter. Rhinovirus infections are often mild but can cause significant discomfort.
- Coronavirus (COVID-19):While COVID-19 cases have declined significantly since the peak of the pandemic, new variants continue to emerge. October 2024 may see a resurgence in cases due to the emergence of a new variant, potentially leading to increased hospitalizations and deaths.
Vaccination and booster doses remain essential for protecting against severe illness.
Emerging Viral Strains and Variants
The emergence of new viral strains and variants is a continuous challenge. In October 2024, there are concerns about:
- Influenza A H3N2:A new sub-lineage of H3N2 influenza is circulating, exhibiting increased transmissibility and potential for causing more severe illness. This variant is likely to contribute to a larger influenza season compared to previous years.
- COVID-19 Omicron Subvariants:Omicron subvariants continue to evolve, with new strains emerging regularly. Some subvariants are exhibiting increased transmissibility and potential for immune evasion, necessitating ongoing surveillance and vaccine development.
2. Symptoms and Transmission
Understanding the symptoms and transmission of prevalent viruses is crucial for early detection, prompt medical attention, and effective prevention strategies. This section provides information on common symptoms, modes of transmission, and prevention tips for each virus.
Common Symptoms and Transmission
The table below Artikels common symptoms, modes of transmission, and prevention tips for prevalent viruses in October 2024.
| Virus | Common Symptoms | Modes of Transmission | Prevention Tips |
|---|---|---|---|
| Influenza (Flu) | Fever, cough, sore throat, runny nose, muscle aches, fatigue, headache | Respiratory droplets from coughing or sneezing, close contact with infected individuals | Get vaccinated annually, wash hands frequently, cover coughs and sneezes, avoid close contact with sick individuals |
| Respiratory Syncytial Virus (RSV) | Runny nose, cough, fever, wheezing, difficulty breathing | Respiratory droplets, close contact with infected individuals, contaminated surfaces | Wash hands frequently, avoid close contact with sick individuals, clean and disinfect surfaces |
| Coronavirus (COVID-19) | Fever, cough, shortness of breath, fatigue, muscle aches, headache, sore throat, loss of taste or smell | Respiratory droplets, close contact with infected individuals, contaminated surfaces, airborne transmission | Get vaccinated and boosted, wear a mask in public indoor settings, wash hands frequently, maintain physical distance, avoid close contact with sick individuals |
| Rhinovirus (Common Cold) | Runny nose, sneezing, sore throat, cough, congestion | Respiratory droplets, close contact with infected individuals, contaminated surfaces | Wash hands frequently, avoid close contact with sick individuals, clean and disinfect surfaces |
Influenza (Flu)
Symptoms
Flu symptoms typically appear 1-4 days after exposure to the virus. The most common symptoms include:
- Fever
- Cough
- Sore throat
- Runny nose
- Muscle aches
- Fatigue
- Headache
Less common symptoms may include:
- Chills
- Vomiting
- Diarrhea
Severe flu infections can lead to complications such as pneumonia, bronchitis, ear infections, and sinus infections.
Transmission
Flu is primarily spread through respiratory droplets produced when an infected person coughs or sneezes. These droplets can travel up to 6 feet and can be inhaled by others.
Flu can also spread through contact with contaminated surfaces, such as doorknobs, phones, or keyboards.
Prevention
The best way to prevent the flu is to get vaccinated annually. The flu vaccine can significantly reduce your risk of getting sick, and even if you do get sick, it can lessen the severity of your illness. Other prevention tips include:
- Washing hands frequently with soap and water for at least 20 seconds, especially after blowing your nose, coughing, or sneezing.
- Covering your mouth and nose with a tissue or your elbow when you cough or sneeze.
- Avoiding close contact with sick individuals.
- Cleaning and disinfecting frequently touched surfaces.
Respiratory Syncytial Virus (RSV)
Symptoms
RSV symptoms typically appear 4-6 days after exposure to the virus. The most common symptoms include:
- Runny nose
- Cough
- Fever
- Wheezing
- Difficulty breathing
In severe cases, RSV can cause bronchiolitis, which is an inflammation of the small airways in the lungs.
Transmission
RSV is primarily spread through respiratory droplets produced when an infected person coughs or sneezes. These droplets can travel up to 6 feet and can be inhaled by others.
RSV can also spread through contact with contaminated surfaces, such as toys, doorknobs, or phones.
Prevention
There is no vaccine for RSV, but there are several ways to prevent its spread:
- Washing hands frequently with soap and water for at least 20 seconds, especially after blowing your nose, coughing, or sneezing.
- Covering your mouth and nose with a tissue or your elbow when you cough or sneeze.
- Avoiding close contact with sick individuals.
- Cleaning and disinfecting frequently touched surfaces.
Symptoms
COVID-19 symptoms typically appear 2-14 days after exposure to the virus. The most common symptoms include:
- Fever
- Cough
- Shortness of breath
- Fatigue
- Muscle aches
- Headache
- Sore throat
- Loss of taste or smell
Some individuals may experience no symptoms at all, while others may develop severe illness, including pneumonia, acute respiratory distress syndrome (ARDS), and multi-organ failure.
Transmission
COVID-19 is primarily spread through respiratory droplets produced when an infected person coughs, sneezes, or talks. These droplets can travel up to 6 feet and can be inhaled by others.
COVID-19 can also spread through contact with contaminated surfaces, such as doorknobs, phones, or keyboards. The virus can also be spread through airborne transmission, which occurs when virus particles remain suspended in the air for longer periods and can travel further than 6 feet.
Prevention
The best way to prevent COVID-19 is to get vaccinated and boosted. The COVID-19 vaccine can significantly reduce your risk of getting sick, and even if you do get sick, it can lessen the severity of your illness. Other prevention tips include:
- Wearing a mask in public indoor settings, especially in crowded or poorly ventilated areas.
- Washing hands frequently with soap and water for at least 20 seconds, especially after blowing your nose, coughing, or sneezing.
- Covering your mouth and nose with a tissue or your elbow when you cough or sneeze.
- Avoiding close contact with sick individuals.
- Maintaining physical distance from others, especially in crowded settings.
- Cleaning and disinfecting frequently touched surfaces.
Rhinovirus (Common Cold)
Symptoms
Cold symptoms typically appear 1-3 days after exposure to the virus. The most common symptoms include:
- Runny nose
- Sneezing
- Sore throat
- Cough
- Congestion
In some cases, a cold can lead to complications such as ear infections, sinus infections, and bronchitis.
Transmission
Rhinovirus is primarily spread through respiratory droplets produced when an infected person coughs or sneezes. These droplets can travel up to 6 feet and can be inhaled by others.
Rhinovirus can also spread through contact with contaminated surfaces, such as doorknobs, phones, or keyboards.
Prevention
There is no vaccine for the common cold, but there are several ways to prevent its spread:
- Washing hands frequently with soap and water for at least 20 seconds, especially after blowing your nose, coughing, or sneezing.
- Covering your mouth and nose with a tissue or your elbow when you cough or sneeze.
- Avoiding close contact with sick individuals.
- Cleaning and disinfecting frequently touched surfaces.
Impact on Public Health

The widespread circulation of these viruses can have significant repercussions on public health, potentially leading to increased hospitalizations, strain on healthcare systems, and economic consequences.
Hospitalizations and Mortality Rates
The potential impact of these viruses on public health is a serious concern. Increased hospitalizations and mortality rates are possible, particularly among vulnerable populations such as the elderly, young children, and individuals with underlying health conditions.
Strain on Healthcare Systems
A surge in viral infections can put a significant strain on healthcare systems. Hospitals and clinics may face challenges in managing the influx of patients, leading to longer wait times, potential staff shortages, and a strain on resources such as beds, ventilators, and medical supplies.
Economic Consequences
Widespread viral infections can have significant economic consequences. Absenteeism from work and school can disrupt businesses and educational institutions, impacting productivity and economic output. The cost of healthcare services, including hospitalizations and treatments, can also strain healthcare budgets and impact overall economic activity.
Vaccination and Treatment Options
The ongoing viral situation in October 2024 underscores the importance of vaccination and effective treatment options. Fortunately, ongoing research and development have yielded significant advancements in both areas.
Available Vaccines and Their Effectiveness
The effectiveness of vaccines against circulating viruses is a crucial aspect of public health preparedness. The current vaccine landscape offers a range of options, each tailored to target specific viral strains.
- Seasonal Flu Vaccine:The seasonal flu vaccine remains a cornerstone of protection against influenza viruses. It is typically updated annually to match the dominant strains circulating during the flu season. The effectiveness of the flu vaccine varies from year to year, but it can significantly reduce the risk of severe illness, hospitalization, and death.
- COVID-19 Vaccines:COVID-19 vaccines have proven to be highly effective in preventing severe illness, hospitalization, and death from the virus. Multiple vaccine platforms, including mRNA and viral vector vaccines, are available. Boosters are recommended to maintain optimal protection against emerging variants.
- Other Viral Vaccines:Vaccines for other viral infections, such as measles, mumps, rubella, and chickenpox, continue to be available and play a crucial role in preventing outbreaks.
Current Treatment Options for Viral Infections
Treatment options for viral infections are constantly evolving. The goal is to alleviate symptoms, prevent complications, and support the body’s natural immune response.
- Antiviral Medications:Antiviral medications work by interfering with the replication of viruses within the body. They are most effective when administered early in the course of an infection. Examples include Tamiflu for influenza and Paxlovid for COVID-19.
- Supportive Care:Supportive care involves measures to manage symptoms and prevent complications. This may include rest, hydration, over-the-counter pain relievers, and fever reducers.
- Immunotherapy:Immunotherapy aims to boost the body’s immune response to fight viral infections. This may involve using antibodies or other immune system-modulating agents.
Ongoing Research and Development
Research and development efforts are continuously underway to develop new and improved vaccines and treatments for viral infections.
- Universal Flu Vaccine:Researchers are working to develop a universal flu vaccine that would provide broad protection against all influenza strains, eliminating the need for annual updates.
- Novel Antiviral Therapies:The development of novel antiviral therapies is an active area of research. These therapies may target different aspects of the viral life cycle, offering new avenues for treatment.
- Pan-Viral Vaccines:Scientists are exploring the possibility of pan-viral vaccines that could protect against a wide range of viruses, including emerging threats.
6. Historical Context
Understanding the historical context of viral outbreaks is crucial for comprehending the current landscape and informing future preparedness strategies. Analyzing past trends and responses provides valuable insights into the evolution of viral behavior, public health interventions, and societal impacts.
Evolution of Viral Trends
Comparing the viral trends in October 2024 to historical data from the past five years reveals a dynamic landscape shaped by factors such as viral evolution, public health measures, and social media dynamics. For instance, the emergence of new viral variants, like the Omicron subvariant BA.5 in 2023, led to a surge in cases and prompted renewed public health concerns.
This trend was reflected in social media discussions, where topics like vaccine efficacy, mask mandates, and travel restrictions dominated online conversations.
Impact of Major Viral Outbreaks
Major viral outbreaks, such as the 1918 Spanish Flu and the 2009 H1N1 pandemic, have profoundly impacted public health and societal structures. These events serve as stark reminders of the potential devastation caused by viral infections and highlight the importance of preparedness and effective response strategies.
Public Health Measures
- During the 1918 Spanish Flu, public health measures focused on isolation, quarantine, and mask mandates. These strategies aimed to limit the spread of the virus by physically separating infected individuals from the healthy population.
- The 2009 H1N1 pandemic saw a more multifaceted approach, including public awareness campaigns, antiviral medication distribution, and school closures. These measures aimed to educate the public about the virus, provide treatment options, and minimize transmission in high-risk settings.
Social and Economic Consequences
- The 1918 Spanish Flu led to widespread disruptions in daily life, including business closures, school shutdowns, and social gatherings. The economic impact was significant, as industries slowed down and unemployment rates rose.
- The 2009 H1N1 pandemic, while less severe than the Spanish Flu, still had notable social and economic consequences. Increased healthcare burden, economic strain, and temporary social isolation were some of the key impacts.
Technological Advancements
- Technological advancements have significantly influenced our understanding and response to viral outbreaks. The development of real-time surveillance systems, advanced diagnostic tools, and rapid communication platforms has enabled faster detection, diagnosis, and public health interventions.
- The use of social media platforms has become an integral part of public health communication during outbreaks, allowing for rapid dissemination of information and public awareness campaigns.
Evolution of Public Health Interventions
The evolution of public health interventions in response to viral outbreaks reflects a continuous process of learning and adaptation. Early interventions focused on isolation, quarantine, and basic hygiene practices. Over time, advancements in medical science and technology have led to the development of more sophisticated strategies, including antiviral medications, vaccines, and advanced surveillance systems.
Comparison of Past and Current Practices
- In the past, public health interventions were often reactive and focused on containing outbreaks once they had emerged. Current practices emphasize proactive measures, including surveillance, early detection, and rapid response mechanisms.
- The development of vaccines and antiviral medications has significantly transformed our ability to prevent and control viral outbreaks. While early interventions relied primarily on non-pharmaceutical measures, current strategies leverage a combination of pharmaceutical and non-pharmaceutical approaches.
Impact of Technological Advancements
Technological advancements have played a pivotal role in enhancing our ability to prevent and control viral outbreaks. The development of real-time surveillance systems, advanced diagnostic tools, and rapid communication platforms has enabled faster detection, diagnosis, and public health interventions. The use of social media platforms has become an integral part of public health communication during outbreaks, allowing for rapid dissemination of information and public awareness campaigns.
7. Global Perspective
Understanding the global spread of a virus is crucial for effective public health interventions and resource allocation. This section examines the global impact of specific viruses, their prevalence and distribution across regions, and the international efforts undertaken to combat outbreaks.
7.1. Viral Spread and Regional Impact
The global impact of a virus can vary significantly depending on factors such as population density, healthcare infrastructure, and socioeconomic conditions.
| Region | Number of Cases | Mortality Rate | Healthcare System Strain | Socioeconomic Impact |
|---|---|---|---|---|
| Region A | [Number] | [Rate] | [Description] | [Description] |
| Region B | [Number] | [Rate] | [Description] | [Description] |
| Region C | [Number] | [Rate] | [Description] | [Description] |
For example, in the case of COVID-19, the impact on different regions varied significantly. In regions with high population density and limited healthcare infrastructure, the virus spread rapidly and overwhelmed healthcare systems, leading to a higher mortality rate and severe socioeconomic consequences.
In contrast, regions with robust healthcare systems and lower population density experienced a slower spread and lower mortality rates.
7.2. Prevalence and Geographic Distribution
The prevalence of a virus can vary greatly across different countries and regions due to factors such as climate, geography, and vaccination rates.
The prevalence of a virus is defined as the proportion of a population that is infected with the virus at a given time.
For instance, dengue fever is prevalent in tropical and subtropical regions with high mosquito populations, while malaria is more common in regions with warm temperatures and high humidity.
- Map:A world map could be used to visualize the prevalence of a specific virus, with color gradients indicating different levels of infection. For example, darker shades could represent areas with higher infection rates, while lighter shades could indicate areas with lower infection rates.
This visual representation would provide a clear picture of the geographic distribution of the virus and help identify areas with high prevalence for targeted interventions.
7.3. International Collaboration and Response
International collaboration is essential for addressing global health threats like viral outbreaks.
- Timeline:A timeline could be used to highlight key milestones in the international response to a specific viral outbreak, such as the declaration of public health emergencies, the development of vaccines and treatments, and international aid and support. This would demonstrate the evolution of the international response and identify areas where collaboration was effective or could be improved.
For example, during the COVID-19 pandemic, international organizations like the World Health Organization (WHO) played a crucial role in coordinating global efforts, sharing information, and providing guidance to countries. The development of vaccines and treatments was also a collaborative effort involving researchers and pharmaceutical companies from around the world.
Future Considerations: Virus Going Around October 2024
The emergence and spread of new viral strains, coupled with the increasing interconnectedness of the global population, pose significant challenges for public health. Understanding and addressing these challenges require a proactive approach that incorporates technological advancements, ongoing research, and robust surveillance systems.
Technological Advancements in Viral Prevention and Management, Virus Going Around October 2024
Technological advancements play a crucial role in mitigating the impact of viral outbreaks. Advancements in areas such as diagnostics, therapeutics, and public health infrastructure can significantly enhance our ability to prevent, detect, and manage viral infections.
- Rapid and Accurate Diagnostics:The development of rapid and accurate diagnostic tests, such as point-of-care tests and molecular diagnostics, enables timely identification of infected individuals, facilitating isolation and contact tracing efforts. Examples include the rapid antigen tests for COVID-19, which have played a significant role in pandemic management.
- Personalized Medicine and Targeted Therapies:Advancements in genomics and personalized medicine allow for tailored therapeutic approaches based on individual genetic profiles and viral strain characteristics. This personalized approach can enhance treatment efficacy and reduce the risk of drug resistance. For instance, the development of antiviral drugs specifically targeting the spike protein of SARS-CoV-2 has proven effective in treating COVID-19.
- Artificial Intelligence (AI) and Machine Learning (ML):AI and ML algorithms can analyze large datasets, identify patterns, and predict potential outbreaks. These technologies can be used to develop early warning systems, optimize resource allocation, and track the spread of viruses. For example, AI-powered surveillance systems can monitor social media posts and news articles for emerging health concerns, providing valuable insights into potential outbreaks.
- Vaccination and Immunotherapy:Advancements in vaccine technology, such as mRNA vaccines, have significantly improved the speed and efficiency of vaccine development. Additionally, research into immunotherapy, which utilizes the body’s immune system to fight infections, holds promise for developing novel treatment strategies.
The Importance of Ongoing Research and Surveillance
Continued research and surveillance are essential for staying ahead of emerging viral threats. Understanding the evolution of viruses, their transmission dynamics, and the development of new strains requires ongoing scientific investigation.
- Viral Evolution and Strain Characterization:Continuous monitoring of viral genomes and their mutations allows researchers to track the emergence of new variants and assess their potential impact on transmissibility, virulence, and vaccine efficacy. This information is crucial for developing effective countermeasures, such as updated vaccines or antiviral treatments.
- Surveillance Systems and Data Analysis:Robust surveillance systems, including laboratory-based testing, case reporting, and data analysis, provide critical insights into the incidence, distribution, and trends of viral infections. This data informs public health interventions, such as targeted vaccination campaigns or social distancing measures.
- Animal Reservoirs and Zoonotic Transmission:Research into zoonotic diseases, which originate in animals and spread to humans, is crucial for understanding the origins of emerging viruses and preventing future outbreaks. This research involves studying animal populations, identifying potential spillover events, and developing strategies to mitigate the risk of zoonotic transmission.
9. Ethical Considerations
The current viral landscape presents a complex ethical landscape, demanding careful consideration of the potential impact of public health measures on individual liberties and societal well-being. Balancing individual autonomy with the collective good necessitates a nuanced approach that prioritizes both individual rights and the protection of public health.
9.1 Vaccine Distribution and Access
The equitable distribution of vaccines is a crucial ethical imperative, ensuring that all individuals have access to life-saving protection. The challenges of achieving this goal are multifaceted, encompassing resource allocation, geographical disparities, and the potential for vaccine nationalism.
- Resource Allocation:Ensuring equitable vaccine distribution necessitates addressing the unequal distribution of resources globally. Wealthier nations often have greater access to vaccines, leaving developing countries with limited access. This disparity raises ethical concerns about fairness and justice in the allocation of life-saving resources.
- Geographic Disparities:Geographical disparities exacerbate the challenge of equitable vaccine distribution. Remote and underserved communities often face logistical barriers to accessing vaccines, highlighting the need for targeted interventions and infrastructure development.
- Vaccine Nationalism:The emergence of vaccine nationalism, where countries prioritize their own citizens for vaccine access, raises ethical concerns about global solidarity and the potential for exacerbating health inequalities. International cooperation and collaboration are essential to ensure equitable vaccine distribution and access.
9.2 Public Health Messaging and Communication
Effective public health messaging is crucial for fostering public trust in vaccines and promoting informed decision-making. However, the potential for misinformation and disinformation poses significant ethical challenges.
- Misinformation and Disinformation:The spread of misinformation and disinformation can erode public trust in vaccines, leading to vaccine hesitancy and undermining public health efforts. Combating misinformation requires a multifaceted approach, including promoting accurate information, addressing public concerns, and leveraging credible sources.
- Fear-Based Messaging:The use of fear-based messaging in public health campaigns can be ethically problematic. While such messaging can be effective in raising awareness, it can also generate anxiety and distrust, potentially leading to negative consequences. Public health messaging should prioritize evidence-based information and promote a sense of empowerment and agency.
- Tailoring Messages to Demographics:Tailoring public health messages to different demographics and cultural contexts can be ethically complex. While it is important to consider cultural sensitivities and ensure accessibility, there is a risk of perpetuating stereotypes or unintentionally reinforcing existing inequalities. A nuanced and inclusive approach is essential to ensure that messaging is culturally appropriate and avoids unintended consequences.
9.3 Individual Liberties vs. Collective Public Health
Balancing individual liberties with the need to protect the collective public health is a fundamental ethical challenge. This tension is particularly evident in the context of public health measures like vaccine mandates, contact tracing apps, and travel restrictions.
- Vaccine Mandates:Vaccine mandates raise ethical concerns about individual autonomy and the right to refuse medical treatment. While such measures can be effective in increasing vaccination rates and protecting the vulnerable, they can also be seen as an infringement on personal liberty.
A careful consideration of the potential benefits and risks is necessary to determine the ethical justification for vaccine mandates.
- Contact Tracing Apps:The use of contact tracing apps raises ethical concerns about privacy and data security. While such apps can be valuable tools for identifying and isolating individuals who may have been exposed to the virus, they also collect personal data that could be misused or compromised.
Transparent data governance and robust privacy protections are essential to ensure the ethical use of contact tracing apps.
- Travel Restrictions:Travel restrictions can be effective in limiting the spread of infectious diseases, but they also raise ethical concerns about freedom of movement and the potential for economic and social harm. Ethical considerations surrounding travel restrictions include the justification for imposing such measures, the potential for discrimination, and the impact on vulnerable populations.
10. Social and Economic Impacts
Viral outbreaks have profound impacts on societies and economies, disrupting daily life, straining healthcare systems, and causing widespread economic disruption. The 2009 H1N1 pandemic serves as a stark reminder of the far-reaching consequences of viral outbreaks, highlighting the interconnectedness of public health, social interactions, and economic stability.
Social Impacts
The social impacts of viral outbreaks are multifaceted, influencing social norms, restricting public gatherings, disproportionately affecting vulnerable populations, and driving the adoption of new technologies for communication and interaction.
- Changes in social norms:Viral outbreaks often lead to significant shifts in social norms, as individuals become more cautious and prioritize health and safety. During the 2009 H1N1 pandemic, for example, people became more aware of hand hygiene, cough etiquette, and the importance of social distancing.
This resulted in increased awareness of personal health practices and a heightened sense of community responsibility.
- Restrictions on public gatherings:Governments often impose restrictions on public gatherings, such as concerts, sporting events, and religious services, to mitigate the spread of the virus. These restrictions can significantly impact social life, limiting opportunities for entertainment, recreation, and spiritual fulfillment. While intended to protect public health, these measures can lead to social isolation and a sense of loss of normalcy.
- Impact on vulnerable populations:Viral outbreaks can disproportionately affect vulnerable populations, such as the elderly, individuals with underlying health conditions, and those with limited access to healthcare. These groups may experience higher rates of infection, severe illness, and mortality. This underscores the importance of targeted public health interventions and social support systems to protect vulnerable populations.
- Use of technology:Viral outbreaks have accelerated the adoption of technology to facilitate social interaction and maintain connections during periods of physical distancing. Teleconferencing, video calls, and social media platforms have become essential tools for staying connected with family, friends, and colleagues, mitigating the social isolation associated with lockdowns and travel restrictions.
Economic Impacts
The economic consequences of viral outbreaks are substantial, impacting businesses, supply chains, employment, and government spending.
- Business closures:Viral outbreaks can force businesses to close temporarily or permanently, leading to significant economic losses. The 2009 H1N1 pandemic, for example, led to widespread closures of restaurants, retail stores, and entertainment venues, resulting in job losses and reduced consumer spending.
- Supply chain disruptions:Viral outbreaks can disrupt global supply chains, leading to shortages of essential goods and services. Production delays, transportation bottlenecks, and labor shortages can contribute to supply chain disruptions, impacting both businesses and consumers.
- Impact on employment:Viral outbreaks can have a devastating impact on employment, leading to job losses and increased unemployment rates. Business closures, reduced consumer spending, and economic uncertainty can all contribute to job losses. The 2009 H1N1 pandemic resulted in a significant increase in unemployment, particularly in industries heavily affected by social distancing measures.
- Government interventions:Governments often implement economic interventions to mitigate the impact of viral outbreaks. These interventions can include financial assistance for businesses, unemployment benefits for workers, and public health measures to support the recovery of the economy. The effectiveness of these interventions depends on their timely implementation and the severity of the outbreak.
Adapting and Mitigating Impacts
Societies have developed strategies to adapt to and mitigate the social and economic impacts of viral outbreaks. These strategies include public health measures, community support networks, government policies, and technological innovations.
- Public health measures:Public health measures, such as vaccination, mask-wearing, hand hygiene, and social distancing, are essential for preventing the spread of viruses and reducing the impact of outbreaks. Effective public health campaigns and robust surveillance systems are crucial for early detection, containment, and mitigation of outbreaks.
- Community support networks:Community support networks play a vital role in providing assistance to those affected by viral outbreaks. Volunteer organizations, community centers, and faith-based groups can offer food assistance, emotional support, and other essential services to individuals and families in need.
- Government policies:Government policies can help to protect vulnerable populations, support businesses, and promote economic recovery. These policies can include financial assistance for businesses, unemployment benefits for workers, and public health measures to prevent the spread of the virus. Government interventions should be tailored to the specific needs of the population and the severity of the outbreak.
- Technological innovations:Technological innovations can help to mitigate the impact of viral outbreaks by facilitating remote work, online education, and virtual healthcare. These innovations can help to maintain social connections, support economic activity, and reduce the spread of the virus.
11. Environmental Factors
The environment plays a crucial role in the emergence, spread, and evolution of viruses. Understanding the intricate relationship between environmental factors and viral outbreaks is vital for developing effective public health strategies.
Environmental Factors Influencing Viral Emergence and Spread
Specific environmental factors, such as temperature, humidity, and air pollution, can significantly influence the emergence and spread of viruses.
- Temperature:Temperature fluctuations can affect viral stability, transmission rates, and the geographic distribution of vectors. For example, warmer temperatures can increase the breeding season and geographic range of mosquitoes, leading to the spread of mosquito-borne viruses like dengue fever and Zika virus.
- Humidity:Relative humidity levels can impact viral survival and transmission. For instance, high humidity can create favorable conditions for the survival of influenza viruses, contributing to their spread.
- Air Pollution:Air pollution, particularly particulate matter, can suppress immune function and increase susceptibility to viral infections. Studies have shown that exposure to high levels of air pollution can be associated with an increased risk of respiratory infections, including those caused by influenza and coronaviruses.
Impact of Climate Change on Viral Transmission
Climate change is altering global weather patterns, creating conditions that can favor the spread of certain viruses.
- Temperature Increases:Rising temperatures can expand the geographic range of vectors, such as mosquitoes, ticks, and rodents, which can transmit viruses to humans. For instance, warmer temperatures have allowed the Aedes aegypti mosquito, which transmits dengue, Zika, and chikungunya viruses, to spread to new areas.
- Precipitation Patterns:Changes in precipitation patterns can create favorable conditions for mosquito breeding, leading to increased mosquito populations and the spread of mosquito-borne diseases.
- Extreme Weather Events:Extreme weather events, such as floods and droughts, can disrupt human populations and create conditions that favor the spread of viruses. For example, floods can displace populations, increasing the risk of outbreaks of waterborne diseases like cholera.
Deforestation and Habitat Fragmentation
Deforestation and habitat fragmentation can disrupt natural ecosystems and increase the risk of zoonotic transmission, where viruses jump from animals to humans.
- Increased Contact:Deforestation and habitat fragmentation can bring humans into closer contact with wild animals, increasing the likelihood of zoonotic spillover events. For example, the destruction of forests can force bats, known to carry a wide range of viruses, into closer proximity with human settlements.
- Environmental Stress:Deforestation and habitat fragmentation can stress animal populations, making them more susceptible to infections and increasing the likelihood of viral transmission.
Research on Environmental Factors and Viral Outbreaks
Ongoing research efforts are investigating the complex link between environmental factors and viral outbreaks.
- Modeling and Simulation:Researchers are using mathematical models and simulations to predict the impact of climate change on the spread of specific viruses.
- Surveillance and Monitoring:Increased surveillance and monitoring efforts are being implemented to track the emergence and spread of viruses in relation to environmental changes.
- Interdisciplinary Collaboration:Interdisciplinary collaboration between epidemiologists, virologists, climatologists, and other experts is crucial for understanding the complex interactions between environmental factors and viral outbreaks.
Environmental Factors and Viral Transmission
| Virus Name | Environmental Factor | Impact on Transmission |
|---|---|---|
| Dengue Fever | Temperature | Increased mosquito breeding and geographic range. |
| Zika Virus | Precipitation | Increased mosquito breeding and transmission. |
| Influenza | Humidity | Increased viral survival and transmission. |
| Hantavirus | Deforestation | Increased contact with rodents and zoonotic transmission. |
| Ebola Virus | Climate Change | Changes in rainfall patterns and temperature can affect the geographic range of fruit bats, a reservoir for Ebola virus. |
Scenario: Novel Virus Emergence in a Region with Environmental Changes
Imagine a novel virus emerging in a region experiencing significant deforestation and climate change. The combination of these factors could have a profound impact on the virus’s evolution, spread, and impact on human health.
- Evolution:The novel virus could evolve to adapt to the changing environmental conditions, potentially becoming more transmissible or virulent.
- Spread:Deforestation could bring humans into closer contact with animal reservoirs of the virus, increasing the risk of zoonotic transmission. Climate change could also create favorable conditions for the virus to spread to new regions.
- Impact on Human Health:The virus could pose a significant threat to human health, particularly in vulnerable populations. The combined effects of deforestation and climate change could exacerbate the impact of the outbreak.
13. Research and Development
The rapid evolution of viral pathogens presents a constant challenge to researchers and public health officials. To effectively combat emerging and re-emerging viral infections, ongoing research and development efforts are crucial to create new vaccines, antiviral therapies, and diagnostic tools.
This section delves into the latest advancements in these areas, exploring the challenges and opportunities associated with developing effective and safe solutions.
13.1 Vaccine Development
The development of vaccines against viral infections is a complex process that involves several stages, from initial research to clinical trials and eventual approval. The goal of vaccine development is to elicit a robust immune response in the recipient, providing protection against future infections.
The effectiveness of a vaccine depends on factors such as its immunogenicity, safety, and scalability.
- Current State of Research and Development: Research and development for vaccines targeting emerging and re-emerging viral infections, such as [specific virus name], is ongoing. Challenges include the rapid evolution of viruses, the need for large-scale clinical trials, and the potential for adverse events.
Opportunities lie in the development of novel vaccine platforms and the use of advanced technologies for vaccine production.
- Effectiveness of Vaccine Platforms: Different vaccine platforms, such as mRNA, viral vector, and protein subunit, have shown varying degrees of effectiveness in eliciting immune responses against viral infections. mRNA vaccines have demonstrated high efficacy and rapid development timelines, but they require specialized storage and distribution.
Viral vector vaccines offer advantages in terms of stability and ease of administration, but they can trigger immune responses against the vector itself. Protein subunit vaccines are generally considered safe, but they may have lower immunogenicity compared to other platforms.
- Novel Vaccine Technologies: Nanoparticle-based vaccines and DNA vaccines are emerging technologies that hold promise for addressing the challenges posed by rapidly evolving viral pathogens. Nanoparticle-based vaccines can deliver antigens more efficiently and target specific immune cells, while DNA vaccines offer the potential for long-lasting immunity.
These technologies are still under development, and further research is needed to evaluate their safety and efficacy.
Antiviral therapies play a crucial role in managing viral infections by targeting specific viral proteins or pathways, inhibiting viral replication and reducing the severity of disease. However, the development of effective antiviral drugs is often hampered by the emergence of drug resistance, a phenomenon that occurs when viruses mutate and develop resistance to existing therapies.
- Mechanisms of Action and Therapeutic Efficacy: Current antiviral drugs used to treat [specific viral infection] have diverse mechanisms of action, including inhibiting viral entry, replication, or release. While these drugs can be effective in reducing viral load and symptoms, they often have limitations, such as potential side effects, drug resistance, and limited efficacy against certain viral strains.
- Development Pipeline of New Antiviral Therapies: The development pipeline for new antiviral therapies is actively progressing, with researchers exploring novel targets and mechanisms of action. These new therapies aim to overcome the limitations of existing drugs, including improved efficacy, reduced side effects, and a lower risk of drug resistance.
- Combination Therapies: Combination therapies, involving the use of multiple antiviral drugs with different mechanisms of action, have proven effective in improving antiviral efficacy and mitigating the emergence of drug resistance. Examples of successful combination regimens include the use of [specific antiviral drug examples] for the treatment of [specific viral infections].
13.3 Diagnostic Tools
Rapid and accurate diagnosis is essential for effective management of viral infections. Diagnostic tools play a critical role in identifying infected individuals, informing treatment decisions, and guiding public health interventions. The performance characteristics of diagnostic tests are crucial for their effectiveness, including sensitivity, specificity, accuracy, time to result, cost, and accessibility.
- Performance Characteristics of Diagnostic Tests: Different diagnostic tests for [specific viral infection] have varying performance characteristics. PCR tests, for example, are highly sensitive and specific but can be time-consuming and require specialized equipment. Rapid antigen tests are faster and more accessible but may have lower sensitivity.
The choice of diagnostic test depends on the specific clinical context and the desired turnaround time.
- Emerging Diagnostic Technologies: Emerging diagnostic technologies, such as CRISPR-based diagnostics and point-of-care testing, hold promise for improving the rapid and accurate detection of viral infections. CRISPR-based diagnostics offer high sensitivity and specificity, while point-of-care testing allows for on-site diagnosis, reducing the need for laboratory analysis.
- Artificial Intelligence and Machine Learning: Artificial intelligence and machine learning are increasingly being used in developing predictive models for viral outbreaks. These models can analyze data from surveillance systems and diagnostic testing to identify patterns and predict the spread of viral infections, aiding in the timely implementation of public health interventions.
13.4 Genomics and Viral Outbreaks
Genomic sequencing and phylogenetic analysis are powerful tools for understanding the evolution and spread of viral pathogens during outbreaks. By analyzing the genetic makeup of viruses, researchers can track their origins, identify mutations, and determine the transmission pathways.
- Genomic Sequencing and Phylogenetic Analysis: Genomic sequencing allows researchers to determine the complete genetic sequence of a virus, while phylogenetic analysis uses this information to reconstruct the evolutionary history of the virus and its relationships to other strains. For example, during the [specific viral outbreak example], genomic sequencing and phylogenetic analysis helped identify the origin of the outbreak, track its spread, and guide public health interventions.
- Genomic Surveillance: Genomic surveillance involves the continuous monitoring of viral genomes to identify emerging threats and guide public health interventions. By tracking viral mutations and changes in genetic diversity, researchers can anticipate the emergence of drug resistance and inform vaccine development strategies.
- Impact of Viral Genetic Diversity: Viral genetic diversity can have a significant impact on vaccine effectiveness and antiviral drug resistance. Viruses constantly evolve, accumulating mutations that can affect their susceptibility to vaccines and antiviral drugs. Ongoing genomic monitoring is essential for understanding the impact of genetic diversity on vaccine and drug efficacy and for adapting public health strategies accordingly.
13.5 Immunomodulatory Agents
Immunomodulatory agents are a class of drugs that can enhance the host immune response to viral infections. These agents work by modulating the immune system, boosting its ability to fight off viral pathogens. Immunomodulatory therapies have the potential to improve patient outcomes and reduce the severity of viral infections.
- Potential of Immunomodulatory Agents: Immunomodulatory agents can enhance the host immune response to viral infections by stimulating the production of antiviral cytokines, increasing the activity of immune cells, and promoting the development of protective antibodies. Examples of immunomodulatory agents include [specific immunomodulatory agent examples].
- Challenges and Opportunities: Developing safe and effective immunomodulatory therapies for viral infections presents challenges, including potential side effects, immune-related complications, and the need for personalized treatment approaches. Opportunities lie in the development of targeted immunomodulatory therapies that specifically enhance the immune response to viral infections without triggering harmful side effects.
- Combination Therapies: Immunomodulatory agents can be used in combination with antiviral therapies to improve patient outcomes and reduce the severity of viral infections. By enhancing the immune response, immunomodulatory agents can augment the effectiveness of antiviral drugs and reduce the risk of drug resistance.
International Collaboration
The global nature of viral threats necessitates international collaboration to effectively address them. Sharing knowledge, resources, and expertise across borders is crucial to contain outbreaks, develop vaccines and treatments, and prevent future pandemics.International collaboration is essential for a multifaceted response to viral outbreaks.
This includes:
Examples of Successful Partnerships
Successful international partnerships have demonstrated the effectiveness of collaborative efforts in combating viral outbreaks. For instance, the Global Fund to Fight AIDS, Tuberculosis and Malaria has played a vital role in providing financial support and coordinating global efforts to combat these diseases.
The World Health Organization (WHO) has also been instrumental in leading international response efforts to outbreaks like Ebola and Zika, providing technical guidance and coordinating global response efforts.
- The Global Fund to Fight AIDS, Tuberculosis and Malaria has raised billions of dollars to support programs in developing countries, resulting in significant progress in reducing HIV/AIDS, tuberculosis, and malaria cases.
- The WHO’s response to the Ebola outbreak in West Africa in 2014-2016 involved coordinating international efforts, providing technical support, and deploying medical personnel to affected countries.
- The development and distribution of COVID-19 vaccines was a remarkable example of international collaboration, with scientists, researchers, and pharmaceutical companies from around the world working together to develop and distribute vaccines in record time.
The Role of International Health Agencies
International health agencies and organizations play a critical role in coordinating global response efforts to viral threats. These agencies provide technical expertise, mobilize resources, and facilitate information sharing between countries. They also work to strengthen national health systems and promote global health security.
- The WHO acts as the leading international health agency, providing guidance, coordinating global response efforts, and monitoring outbreaks.
- The Centers for Disease Control and Prevention (CDC) in the United States provides expertise and technical support to countries around the world in areas such as disease surveillance, outbreak investigation, and public health preparedness.
- The European Centre for Disease Prevention and Control (ECDC) plays a similar role in Europe, coordinating disease surveillance and response efforts across the continent.
Closing Notes
As we navigate the ever-evolving world of viruses, staying informed and taking proactive measures is essential. By understanding the viruses circulating in our communities, practicing good hygiene, and staying up-to-date on vaccination recommendations, we can help protect ourselves and contribute to a healthier society.
Remember, vigilance and knowledge are our greatest allies in the face of viral threats.
FAQ Insights
What are the most common symptoms of a viral infection?
Common symptoms of viral infections include fever, cough, sore throat, runny nose, fatigue, headache, and muscle aches. However, specific symptoms can vary depending on the virus.
How long does a typical viral infection last?
The duration of a viral infection can vary greatly depending on the virus, individual health, and other factors. Most viral infections resolve within a few days to a week, but some can linger for several weeks or even months.
Is there a specific treatment for all viral infections?
There is no single cure for all viral infections. Treatment typically focuses on managing symptoms and supporting the body’s natural immune response. Antiviral medications may be prescribed in some cases, depending on the specific virus.